Risk factors and chronic diseases often get more attention among the middle-age and elderly population. And rightly so, since that?s when the manifestations of chronic diseases start to show up, and when people get reminded about their chronological age.? An integral component of successful aging (also known as healthy aging) is the freedom of physical disabilities and debilitating chronic diseases 1-3. While it is true that it is never too late to become health conscious and reap the benefits of a healthy lifestyle 4,5, the fact remains that the sooner we start the better off we will be as we get older. If you are in your 20s or 30s, or have kids, read on?
This is a long article, so here are some jump-to links:
Appearances are deceptive
Risk factor prevalence
Health risk screening
Bottom Line
References
To navigate back up, just hit ctrl+home. Oki, roll up your sleeves and off we go?.
A life course approach to successful aging
Chronic diseases are the largest threat to a long and vital life. A prevention-oriented life course approach starting in childhood and young adolescence is critical to establishing and maintaining health throughout life 6-8. ?And thereby lays the ground for successful aging as we get older 2,9,10.
Attitudes and risk perceptions among young adults
Adolescents and young adults often underestimate the negative consequences of their personal behaviors and habits, and have unrealistic optimism of vulnerability 11-15. This is especially true for heart/cardiovascular disease risk 11,16-19. This ?I am young and don?t have to worry? or ?it won?t happen to me? attitude, however, can have serious impact on lifestyle choices and future health outcomes.
Denial is putting a large majority of the population at undue high risk. The Heart and Stroke Foundation found that while people are aware of the importance of addressing their risk factors, most have a false sense of security that is cutting their lives short 20. People consistently overestimate their own healthy behaviors:
- Almost 90% of rate themselves as healthy. The reality is that 9 out of 10 s have at least one risk factor for heart disease and stroke.
- Only about a third said they are not physically active or don?t eat a minimum of five servings of vegetables and fruit per day. The reality is about half don?t meet the physical activity and healthy eating recommendations.
- 18% of adults say they are obese. The reality is that almost one quarter ? 25% ? are obese.
Among people with blood lipid abnormalities, only 35% are aware that they have it 21, and many don?t even know their blood pressure 22. This huge chasm between perception and reality could be fatal.
Appearances are deceptive
The fact that appearances are deceptive is true in many areas in life, and most of us have experienced it first hand in social interactions. However, it is also true when it comes to risk factors for chronic diseases.
 While visible risk status, like body fatness, diet and exercise, is a good marker for other non-visible risk factors (like blood pressure, diabetes, respiratory function), they don?t always go together. It has been documented in both the lay and medical arena that even people with no visible risk factors die prematurely, and conversely that sometimes people who show visible risk factors live longer than expected 23. A study that specifically investigated these ?anomalous deaths? and ?unwarranted survivors? concluded that theses aberrant observations can be explained by the presence or lack of non-visible risk factors 24. While the low visible risk status group in general lived longer than the high visible risk status group, within each group there were notable survival differences. Premature deaths in the low visible risk status group were explained by the presence of non-visible risk factors, and longer than expected survival in the high visible risk status group was due to absence of non-visible risk factors 24.
While visible risk status, like body fatness, diet and exercise, is a good marker for other non-visible risk factors (like blood pressure, diabetes, respiratory function), they don?t always go together. It has been documented in both the lay and medical arena that even people with no visible risk factors die prematurely, and conversely that sometimes people who show visible risk factors live longer than expected 23. A study that specifically investigated these ?anomalous deaths? and ?unwarranted survivors? concluded that theses aberrant observations can be explained by the presence or lack of non-visible risk factors 24. While the low visible risk status group in general lived longer than the high visible risk status group, within each group there were notable survival differences. Premature deaths in the low visible risk status group were explained by the presence of non-visible risk factors, and longer than expected survival in the high visible risk status group was due to absence of non-visible risk factors 24.
Therefore, even if your appearance shows a low risk status, it is important that you still keep track of your invisible risk parameters by getting your regular blood work and health checkups.
Risk factor prevalence
Today very few Americans are at low risk for heart disease. Approximately 78% of adults aged 20-80 years alive today in the United States are candidates for at least one prevention activity 25. Over 55% of young adults have at least one cardiovascular disease risk factor, and over 37% reported having two or more 26.
According to the National Center for Health Statistics, half of American adults have one or more of the three major risk factors: dyslipidemia (abnormal amounts of lipids, lipoproteins and sub-fractions in the blood), high blood pressure, or diabetes 27.? The National Center for Health Statistics also estimates that 15% of adults having one of more of these three risk factors but remain undiagnosed and hence untreated 27.? Recent updates show the following prevalence rates 28-30:
68% overweight or obese
59% abstaining from any vigorous activity
34% hypertension (high blood pressure)
32% pediatric obesity or overweight
36% pre-diabetes in adults over 20 years of age; 50% in those over 65 years of age
34% metabolic syndrome
27% undiagnosed diabetes
21.2% tobacco use
11.2% of adults with both pre-hypertension and pre-diabetes
Among young adults aged 18-39 years, only 20% meet low risk criteria, and almost 60% have high levels of at least one risk factor 31. In young adult and middle-aged populations, aged 18 to 59 years, only 5-10% have a low health risk status 32.
If everyone received th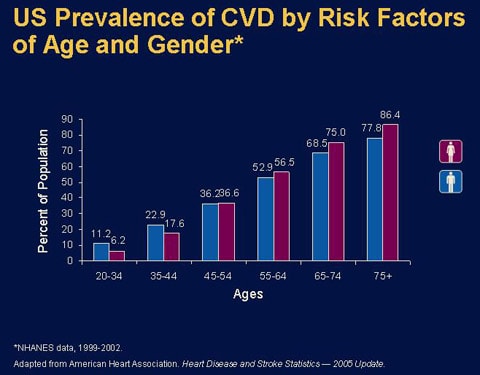 e activities for which they are eligible, heart attacks and strokes would be reduced by 63% and 31%, respectively 25. Of the specific prevention activities, the greatest benefits to the US population come from controlling pre-diabetes, weight reduction in obese individuals, lowering blood pressure, and improving blood lipids 25.
e activities for which they are eligible, heart attacks and strokes would be reduced by 63% and 31%, respectively 25. Of the specific prevention activities, the greatest benefits to the US population come from controlling pre-diabetes, weight reduction in obese individuals, lowering blood pressure, and improving blood lipids 25.
Thus, there is a widespread failure of people to accept disease risks that aren?t obvious and are asymptomatic 33. This, coupled with the enormously high risk factor prevalence in the general public, provides a good rationale to regularly do health checkups, and to start doing so at an early age 34. The fact that risk factor control in adults and elderly reduces, but doesn?t eliminate disease 35 further underscores the importance of early monitoring, prevention and intervention. What?s especially disturbing is that even doctors often underestimate their patient?s risk and are ignorant of risk factors they feel don?t belong to their special medical area 87-90 .? So put your foot down if your physician gives you a clean bill of health without running any comprehensive labs tests.
Health risk screening
Health risk screening is the practice of regularly doing health check-ups even in the absence of manifest disease or disability.
The high prevalence of pre-diabetes and undiagnosed diabetes is especially alarming since elevated fasting blood glucose levels even within the ?normal? range greatly increase the risk for development of full-blown type 2 diabetes 36, stomach cancer 37, and heart attack 38. Fasting blood glucose values in the upper normal range are an important independent predictor of cardiovascular death even in non-diabetic apparently healthy people 39.

A mounting body of evidence shows that high after-meal blood glucose spikes inflict as much or more damage than high fasting blood sugar 40,41. Among individuals with ?normal? blood sugar readings, heart attack risk increases by 58% for a 21 mg/dl increase in after-meal blood sugar level 38. Thus, including
2-h after-meal glucose tests improves the predictive ability to identify non-diabetic individuals at increased risk of cardiovascular death 42. The good news is that many interventions that reduce blood sugar also lower insulin 43, LDL 44-46, triglycerides 44,47-50, and CRP (C-reactive protein, see below) 51, obesity 49,50,52,53 and increase HDL 53, and thereby slash the risk of vascular disease 54, cancer 55,56, dementia 57,58 and many other degenerative disorders.
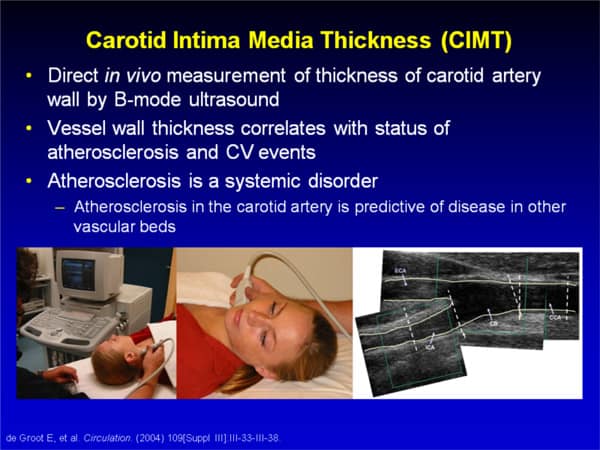
Chronic disease develops and progresses silently for many years before it strikes a clinical manifestation. This is especially true for atherosclerotic diseases such as coronary heart disease, stroke, and peripheral artery disease, which are major health threats. While atherosclerotic complications don?t show up until middle-age or later, the atherosclerotic inducing process begins already in childhood, and has an incubation period of decades and progresses throughout an individual?s lifetime 59-64.
The development of early stages of atherosclerosis in children and adolescents is a function of the same traditional risk factors that affect adults. Worsening of risk factors accelerates the process, and their improvement slows or is even capable of reversing it. The longer the exposure to, and the greater the intensity of the risk factors involved, the higher the atherosclerotic burden will become 64,65.
Significant raised atherosclerotic lesions increase rapidly in prevalence and extent during the 15- to 34-year age span. Therefore, primary prevention of atherosclerosis, in contrast to primary prevention of clinically manifest heart/vascular disease, must begin in childhood or adolescence 66. It was recently found that childhood risk factor measurements obtained at or after 9 years of age are strongly predictive of subclinical atherosclerosis in adulthood 67.
Another study found that dyslipidemia also has consequences during young adulthood. To assess whether non-optimal blood lipid levels during young adulthood cause atherosclerotic changes that persist into middle age, young men and women age 18 to 30 years were followed for 20 years 68. It was found that a whopping 87% had non-optimal baseline levels of LDL cholesterol (over 2.59 mmol/L or over 100 mg/dL), HDL cholesterol (below 1.55 mmol/L or below 60 mg/dL), or triglycerides (over 1.70 mmol/L or over 150 mg/dL) during young adulthood. Coronary calcium (a strong predictor of future coronary heart disease) prevalence 20 years later was 8% in participants who maintained an optimal blood lipid profile, compared to 44% in participants with who did not 68. Both LDL and HDL cholesterol levels were independently associated with coronary calcium, even after participants who were receiving lipid-lowering medications or had clinically abnormal lipid levels were excluded 68. This study shows that even moderate deviations from an optimal blood lipid profile has a significant and long-lasting impact on coronary atherosclerosis in middle-age.
Carotid artery intima-media thickness (CIMT) is a marker of preclinical ?silent? atherosclerosis 69, and ?cardiovascular risk factors during childhood predicts increased CIMT 20 years later 70-73. A recent study examined whether childhood and adolescent (3-18 years of age) risk factors are associated with CIMT progression independent of current, adulthood risk factors 74. After an extended 27 year follow-up with repeated CIMT measurements, it was found that exposure to risk factors in childhood was associated with increased CIMT progression rate in adulthood 74. The childhood risk score, reflecting the composite load of youth risk exposure, was associated with IMT progression even after taking into account the current risk score. When the effects of individual risk variables were assessed, frequent fruit consumption and high physical activity in childhood remained associated with lower adult CIMT progression 74. These observations indicate that children with risk factors have increased atherosclerosis progression rate in adulthood and support the idea that atherosclerosis prevention by means of life style are effective when initiated in childhood 75.
In contrast to childhood life-style variables, the associations of childhood blood lipid values and fatness with CIMT progression became non-significant when adjusted for current adult risk factor levels. Thus, although a composite childhood risk burden was independently associated with CIMT progression, the effects of these specific risk factors lost their significance after the adjustment for adult values. The greater relative importance of adult lipid levels and obesity when compared with those in childhood is also supported by the observation that favorable changes in lipid profile and obesity status from childhood to adulthood were associated with slower atherosclerosis progression. For example, in subjects with low HDL/LDL cholesterol ratio in childhood, only those with low ratio also in adulthood had increased CIMT progression in adulthood. Similarly, obese youths who became lean adults had slower CIMT progression than persistently obese subjects. These findings suggest that it is not too late to start interventions targeting blood lipids and obesity during transition from youth to adulthood to reduce progression of atherosclerosis.
The strong association between coronary heart disease and unfavorable blood lipid profiles has often overshadowed the effects of the non-lipid risk factors like obesity, and diabetes, impaired glucose tolerance, high blood pressure and smoking. It has even led to questioning the importance of these risk factors in the presence of a favorable lipoprotein profile. In a study that investigated the impact of these non-lipid risk factors in young adults, 15 to 34 years of age, with optimal blood lipid profiles, it was found that all of them caused atherosclerotic lesions despite the presence of optimal blood lipid profiles 76. This finding underscores the need to control all cardiovascular risk factors 76.
Another important non-lipid risk factor is CRP (C-reactive protein), an inflammatory marker that can flag atherosclerosis and impending heart disease 77-79. CRP predicts the progression of carotid atherosclerosis in both the middle-aged and elderly (40-70 year old)80, and in young adults (aged 24 to 43 years) 81. In young adults, CRP has independent association with CIMT progression 81, which provides a rationale to screen CRP levels as well, in addition to traditional lipid risk factors. Recent accumulating evidence is showing that CRP is no longer regarded as merely an indicator of cardiovascular risk, but increasingly considered a direct partaker in the development of atherosclerotic cardiovascular disease 82. Thus, rest assured we will hear more about CRP reducing interventions in the near future.
Bottom line
Even if you think your health is good and you aren?t suffering today, don?t take your current health status for granted. Many invisible risk factors can hide behind the surface. Do you really know what your blood pressure, HDL and fasting blood sugar is? And what about C-reactive protein (CRP), the ?new? risk factor which has been shown to be a stronger predictor of cardiovascular events than the infamous LDL (the ?bad? cholesterol) 83? Most people don?t know their invisible risk factors; make sure not to be one of them. Regular health screening and follow-ups are a prerequisite for successful aging.
 While it is true that some of the negative effects of early life influences can effectively be overcome by current healthier behaviors 84, the way one arrives at middle age sets the stage for the years to follow 85. And how well we fare at middle age is in turn determined by how we lived in young adulthood, and even influenced by our childhood years.
While it is true that some of the negative effects of early life influences can effectively be overcome by current healthier behaviors 84, the way one arrives at middle age sets the stage for the years to follow 85. And how well we fare at middle age is in turn determined by how we lived in young adulthood, and even influenced by our childhood years.
Here?s the rationale for regular health screening even in apparently healthy young individuals and children over 9 years:
- The high prevalence of risk factors, both visible and invisible.
- The largest killer, cardiovascular diseases, start to develop silently early in life.
- Most of us have a tendency to greatly underestimate our own health risks.
- Physiological processes that lay the ground for chronic diseases, especially cardiovascular diseases, start early in life. The health status of children aged 9 years or older will have impact on later life health outcomes.
The sooner risk factors are detected and treated, and the more years of our lives that we spend engaging in healthy lifestyle behaviors, the greater our odds for aging successfully and staying vital up to old age. Don?t jeopardize the quality and length of your life by living in denial; take action now and schedule your blood work exam to track your invisible risk factors. See it as an investment in your and your family?s health and happiness. While there will always be exceptions, overall there is truth in ??the older you get, the healthier you have been? 86. Take action now to gain control of your aging destiny!
About Monica Mollica > www.trainergize.com
 Monica Mollica has a Bachelor?s and Master?s degree in Nutrition from the University of Stockholm, Sweden, and is an ISSA Certified Personal Trainer. She works a dietary consultant, health journalist and writer for www.BrinkZone.com, and is also a web designer and videographer.
Monica Mollica has a Bachelor?s and Master?s degree in Nutrition from the University of Stockholm, Sweden, and is an ISSA Certified Personal Trainer. She works a dietary consultant, health journalist and writer for www.BrinkZone.com, and is also a web designer and videographer.
Monica has admired and been fascinated by muscular and sculptured strong athletic bodies since childhood, and discovered bodybuilding as an young teenager. Realizing the importance of nutrition for maximal results in the gym, she went for a BSc and MSc with a major in Nutrition at the University.
During her years at the University she was a regular contributor to the Swedish bodybuilding magazine BODY, and she has published the book (in Swedish) ?Functional Foods for Health and Energy Balance?, and authored several book chapters in Swedish publications.
It was her insatiable thirst for knowledge and scientific research in the area of bodybuilding and health that brought her to the US. She has completed one semester at the PhD-program ?Exercise, Nutrition and Preventive Health? at Baylor University Texas, at the department of Health Human Performance and Recreation, and worked as an ISSA certified personal trainer. Today, Monica is sharing her solid experience by doing dietary consultations and writing about topics related to health, fitness, bodybuilding, anti-aging and longevity.
References:
1. McLaughlin SJ, Jette AM, Connell CM. An Examination of Healthy Aging Across a Conceptual Continuum: Prevalence Estimates, Demographic Patterns, and Validity. The journals of gerontology. Series A, Biological sciences and medical sciences. Feb 24 2012.
2. Rowe JW, Kahn RL. Human aging: usual and successful. Science. Jul 10 1987;237(4811):143-149.
3. Rowe JW, Kahn RL. Successful aging and disease prevention. Advances in renal replacement therapy. Jan 2000;7(1):70-77.
4. Morley JE, Flaherty JH. It?s never too late: health promotion and illness prevention in older persons. The journals of gerontology. Series A, Biological sciences and medical sciences. Jun 2002;57(6):M338-342.
5. Minkler M, Schauffler H, Clements-Nolle K. Health promotion for older Americans in the 21st century. American journal of health promotion : AJHP. Jul-Aug 2000;14(6):371-379.
6. Dwyer J. Starting down the right path: nutrition connections with chronic diseases of later life. The American journal of clinical nutrition. Feb 2006;83(2):415S-420S.
7. Darnton-Hill I, Nishida C, James WP. A life course approach to diet, nutrition and the prevention of chronic diseases. Public health nutrition. Feb 2004;7(1A):101-121.
8. Hayman LL, Helden L, Chyun DA, Braun LT. A life course approach to cardiovascular disease prevention. European journal of cardiovascular nursing : journal of the Working Group on Cardiovascular Nursing of the European Society of Cardiology. Jul 2011;10 Suppl 2:S20-31.
9. Rowe JW. Health care of the elderly. The New England journal of medicine. Mar 28 1985;312(13):827-835.
10. Evert J, Lawler E, Bogan H, Perls T. Morbidity profiles of centenarians: survivors, delayers, and escapers. The journals of gerontology. Series A, Biological sciences and medical sciences. Mar 2003;58(3):232-237.
11. Avis NE, Smith KW, McKinlay JB. Accuracy of perceptions of heart attack risk: what influences perceptions and can they be changed? American journal of public health. Dec 1989;79(12):1608-1612.
12. Millstein SG, Petersen AC, Nightingale EO. Promoting the Health of Adolescents: Oxford University Press; 1993.
13. Weinstein ND. Unrealistic optimism about susceptibility to health problems. Journal of behavioral medicine. Dec 1982;5(4):441-460.
14. Weinstein ND. Why it won?t happen to me: perceptions of risk factors and susceptibility. Health psychology : official journal of the Division of Health Psychology, American Psychological Association. 1984;3(5):431-457.
15. Weinstein ND. Unrealistic optimism about susceptibility to health problems: conclusions from a community-wide sample. Journal of behavioral medicine. Oct 1987;10(5):481-500.
16. Niknian M, McKinlay SM, Rakowski W, Carleton RA. A comparison of perceived and objective CVD risk in a general population. American journal of public health. Dec 1989;79(12):1653-1654.
17. Green JS, Grant M, Hill KL, Brizzolara J, Belmont B. Heart disease risk perception in college men and women. Journal of American college health : J of ACH. Mar 2003;51(5):207-211.
18. Homko CJ, Santamore WP, Zamora L, et al. Cardiovascular disease knowledge and risk perception among underserved individuals at increased risk of cardiovascular disease. The Journal of cardiovascular nursing. Jul-Aug 2008;23(4):332-337.
19. Dearborn JL, McCullough LD. Perception of risk and knowledge of risk factors in women at high risk for stroke. Stroke; a journal of cerebral circulation. Apr 2009;40(4):1181-1186.
20. Heart and Stroke Foundation. Report on Canadians? Health. Denial is putting Canadians at high risk of cutting their lives short. . 2011. http://www.heartandstroke.com/site/c.ikIQLcMWJtE/b.6520045/k.BB7E/2011_Report__Denial_cutting_lives_short.htm.
21. Ford ES, Mokdad AH, Giles WH, Mensah GA. Serum total cholesterol concentrations and awareness, treatment, and control of hypercholesterolemia among US adults: findings from the National Health and Nutrition Examination Survey, 1999 to 2000. Circulation. May 6 2003;107(17):2185-2189.
22. Pearson TA. The prevention of cardiovascular disease: have we really made progress? Health Aff (Millwood). Jan-Feb 2007;26(1):49-60.
23. Frankel S, Davison C, Smith GD. Lay epidemiology and the rationality of responses to health education. The British journal of general practice : the journal of the Royal College of General Practitioners. Oct 1991;41(351):428-430.
24. McConnachie A, Hunt K, Emslie C, Hart C, Watt G. ?Unwarranted survivals? and ?anomalous deaths? from coronary heart disease: prospective survey of general population. BMJ. Dec 22-29 2001;323(7327):1487-1491.
25. Kahn R, Robertson RM, Smith R, Eddy D. The impact of prevention on reducing the burden of cardiovascular disease. Circulation. Jul 29 2008;118(5):576-585.
26. Services UDoHaH. National Center for Health Statistics. Health, United States, 2010. 2010. http://www.cdc.gov/nchs/data/hus/hus10.pdf. Accessed March 5, 2012.
27. Fryar CD, Hirsch R, Eberhardt MS, Yoon SS, Wright JD. Hypertension, high serum total cholesterol, and diabetes: Racial and ethnic prevalence differences in US adults, 1999?2006. . NCHS data brief, no 36. 2010. http://www.cdc.gov/nchs/default.htm. Accessed March 5, 2012.
28. Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999-2008. JAMA : the journal of the American Medical Association. Jan 20 2010;303(3):235-241.
29. Lloyd-Jones D, Adams R, Carnethon M, et al. Heart disease and stroke statistics?2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. Jan 27 2009;119(3):480-486.
30. Lloyd-Jones DM, Hong Y, Labarthe D, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association?s strategic Impact Goal through 2020 and beyond. Circulation. Feb 2 2010;121(4):586-613.
31. Daviglus ML, Stamler J, Pirzada A, et al. Favorable cardiovascular risk profile in young women and long-term risk of cardiovascular and all-cause mortality. JAMA : the journal of the American Medical Association. Oct 6 2004;292(13):1588-1592.
32. Stamler J, Stamler R, Neaton JD, et al. Low risk-factor profile and long-term cardiovascular and noncardiovascular mortality and life expectancy: findings for 5 large cohorts of young adult and middle-aged men and women. JAMA : the journal of the American Medical Association. Dec 1 1999;282(21):2012-2018.
33. Janz NK, Becker MH. The Health Belief Model: a decade later. Health education quarterly. Spring 1984;11(1):1-47.
34. McGill HC, Jr., Herderick EE, McMahan CA, et al. Atherosclerosis in youth. Minerva pediatrica. Oct 2002;54(5):437-447.
35. McGill HC, Jr., McMahan CA, Gidding SS. Preventing heart disease in the 21st century: implications of the Pathobiological Determinants of Atherosclerosis in Youth (PDAY) study. Circulation. Mar 4 2008;117(9):1216-1227.
36. Kato M, Noda M, Suga H, Matsumoto M, Kanazawa Y. Fasting plasma glucose and incidence of diabetes ? implication for the threshold for impaired fasting glucose: results from the population-based Omiya MA cohort study. Journal of atherosclerosis and thrombosis. 2009;16(6):857-861.
37. Yamagata H, Kiyohara Y, Nakamura S, et al. Impact of fasting plasma glucose levels on gastric cancer incidence in a general Japanese population: the Hisayama study. Diabetes care. Apr 2005;28(4):789-794.
38. Gerstein HC, Pais P, Pogue J, Yusuf S. Relationship of glucose and insulin levels to the risk of myocardial infarction: a case-control study. Journal of the American College of Cardiology. Mar 1999;33(3):612-619.
39. Bjornholt JV, Erikssen G, Aaser E, et al. Fasting blood glucose: an underestimated risk factor for cardiovascular death. Results from a 22-year follow-up of healthy nondiabetic men. Diabetes care. Jan 1999;22(1):45-49.
40. Monnier L, Colette C. Glycemic variability: should we and can we prevent it? Diabetes care. Feb 2008;31 Suppl 2:S150-154.
41. Monnier L, Colette C, Owens DR. Glycemic variability: the third component of the dysglycemia in diabetes. Is it important? How to measure it? Journal of diabetes science and technology. Nov 2008;2(6):1094-1100.
42. Lin HJ, Lee BC, Ho YL, et al. Postprandial glucose improves the risk prediction of cardiovascular death beyond the metabolic syndrome in the nondiabetic population. Diabetes care. Sep 2009;32(9):1721-1726.
43. Behall KM, Scholfield DJ, Hallfrisch JG, Liljeberg-Elmstahl HG. Consumption of both resistant starch and beta-glucan improves postprandial plasma glucose and insulin in women. Diabetes care. May 2006;29(5):976-981.
44. Sood N, Baker WL, Coleman CI. Effect of glucomannan on plasma lipid and glucose concentrations, body weight, and blood pressure: systematic review and meta-analysis. The American journal of clinical nutrition. Oct 2008;88(4):1167-1175.
45. Ngondi JL, Oben JE, Minka SR. The effect of Irvingia gabonensis seeds on body weight and blood lipids of obese subjects in Cameroon. Lipids in health and disease. 2005;4:12.
46. Anderson JW, Allgood LD, Turner J, Oeltgen PR, Daggy BP. Effects of psyllium on glucose and serum lipid responses in men with type 2 diabetes and hypercholesterolemia. The American journal of clinical nutrition. Oct 1999;70(4):466-473.
47. Nizami F, Farooqui MS, Munir SM, Rizvi TJ. Effect of fiber bread on the management of diabetes mellitus. Journal of the College of Physicians and Surgeons?Pakistan : JCPSP. Nov 2004;14(11):673-676.
48. Hanefeld M, Cagatay M, Petrowitsch T, Neuser D, Petzinna D, Rupp M. Acarbose reduces the risk for myocardial infarction in type 2 diabetic patients: meta-analysis of seven long-term studies. European heart journal. Jan 2004;25(1):10-16.
49. Udani J, Hardy M, Madsen DC. Blocking carbohydrate absorption and weight loss: a clinical trial using Phase 2 brand proprietary fractionated white bean extract. Alternative medicine review : a journal of clinical therapeutic. Mar 2004;9(1):63-69.
50. Barrett ML, Udani JK. A proprietary alpha-amylase inhibitor from white bean (Phaseolus vulgaris): a review of clinical studies on weight loss and glycemic control. Nutrition journal. 2011;10:24.
51. Derosa G, Maffioli P, Ferrari I, et al. Acarbose actions on insulin resistance and inflammatory parameters during an oral fat load. European journal of pharmacology. Jan 25 2011;651(1-3):240-250.
52. Ebbeling CB, Leidig MM, Sinclair KB, Hangen JP, Ludwig DS. A reduced-glycemic load diet in the treatment of adolescent obesity. Archives of pediatrics & adolescent medicine. Aug 2003;157(8):773-779.
53. Maki KC, Rains TM, Kaden VN, Raneri KR, Davidson MH. Effects of a reduced-glycemic-load diet on body weight, body composition, and cardiovascular disease risk markers in overweight and obese adults. The American journal of clinical nutrition. Mar 2007;85(3):724-734.
54. Vasdev S, Gill V, Singal P. Role of advanced glycation end products in hypertension and atherosclerosis: therapeutic implications. Cell biochemistry and biophysics. 2007;49(1):48-63.
55. Wu WT, Chen HL. Effects of konjac glucomannan on putative risk factors for colon carcinogenesis in rats fed a high-fat diet. Journal of agricultural and food chemistry. Feb 9 2011;59(3):989-994.
56. Bravi F, Edefonti V, Bosetti C, et al. Nutrient dietary patterns and the risk of colorectal cancer: a case-control study from Italy. Cancer causes & control : CCC. Nov 2010;21(11):1911-1918.
57. Yaffe K, Blackwell T, Whitmer RA, Krueger K, Barrett Connor E. Glycosylated hemoglobin level and development of mild cognitive impairment or dementia in older women. The journal of nutrition, health & aging. Jul-Aug 2006;10(4):293-295.
58. Xu W, Qiu C, Winblad B, Fratiglioni L. The effect of borderline diabetes on the risk of dementia and Alzheimer?s disease. Diabetes. Jan 2007;56(1):211-216.
59. Enos WF, Holmes RH, Beyer J. Coronary disease among United States soldiers killed in action in Korea; preliminary report. Journal of the American Medical Association. Jul 18 1953;152(12):1090-1093.
60. McGill HC, Jr., McMahan CA. Determinants of atherosclerosis in the young. Pathobiological Determinants of Atherosclerosis in Youth (PDAY) Research Group. The American journal of cardiology. Nov 26 1998;82(10B):30T-36T.
61. Newman WP, 3rd, Freedman DS, Voors AW, et al. Relation of serum lipoprotein levels and systolic blood pressure to early atherosclerosis. The Bogalusa Heart Study. The New England journal of medicine. Jan 16 1986;314(3):138-144.
62. Berenson GS, Srinivasan SR, Bao W, Newman WP, 3rd, Tracy RE, Wattigney WA. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. The Bogalusa Heart Study. The New England journal of medicine. Jun 4 1998;338(23):1650-1656.
63. Kavey RE, Daniels SR, Lauer RM, Atkins DL, Hayman LL, Taubert K. American Heart Association guidelines for primary prevention of atherosclerotic cardiovascular disease beginning in childhood. Circulation. Mar 25 2003;107(11):1562-1566.
64. McMahan CA, Gidding SS, Viikari JS, et al. Association of Pathobiologic Determinants of Atherosclerosis in Youth risk score and 15-year change in risk score with carotid artery intima-media thickness in young adults (from the Cardiovascular Risk in Young Finns Study). The American journal of cardiology. Oct 1 2007;100(7):1124-1129.
65. Sniderman AD, Lawler PR, Williams K, Thanassoulis G, de Graaf J, Furberg CD. The causal exposure model of vascular disease. Clin Sci (Lond). Apr 2012;122(8):369-373.
66. Strong JP, Malcom GT, McMahan CA, et al. Prevalence and extent of atherosclerosis in adolescents and young adults: implications for prevention from the Pathobiological Determinants of Atherosclerosis in Youth Study. JAMA : the journal of the American Medical Association. Feb 24 1999;281(8):727-735.
67. Juonala M, Magnussen CG, Venn A, et al. Influence of age on associations between childhood risk factors and carotid intima-media thickness in adulthood: the Cardiovascular Risk in Young Finns Study, the Childhood Determinants of Adult Health Study, the Bogalusa Heart Study, and the Muscatine Study for the International Childhood Cardiovascular Cohort (i3C) Consortium. Circulation. Dec 14 2010;122(24):2514-2520.
68. Pletcher MJ, Bibbins-Domingo K, Liu K, et al. Nonoptimal lipids commonly present in young adults and coronary calcium later in life: the CARDIA (Coronary Artery Risk Development in Young Adults) study. Annals of internal medicine. Aug 3 2010;153(3):137-146.
69. Lorenz MW, Markus HS, Bots ML, Rosvall M, Sitzer M. Prediction of clinical cardiovascular events with carotid intima-media thickness: a systematic review and meta-analysis. Circulation. Jan 30 2007;115(4):459-467.
70. Magnussen CG, Venn A, Thomson R, et al. The association of pediatric low- and high-density lipoprotein cholesterol dyslipidemia classifications and change in dyslipidemia status with carotid intima-media thickness in adulthood evidence from the cardiovascular risk in Young Finns study, the Bogalusa Heart study, and the CDAH (Childhood Determinants of Adult Health) study. Journal of the American College of Cardiology. Mar 10 2009;53(10):860-869.
71. Davis PH, Dawson JD, Riley WA, Lauer RM. Carotid intimal-medial thickness is related to cardiovascular risk factors measured from childhood through middle age: The Muscatine Study. Circulation. Dec 4 2001;104(23):2815-2819.
72. Li S, Chen W, Srinivasan SR, et al. Childhood cardiovascular risk factors and carotid vascular changes in adulthood: the Bogalusa Heart Study. JAMA : the journal of the American Medical Association. Nov 5 2003;290(17):2271-2276.
73. Koskinen J, Kahonen M, Viikari JS, et al. Conventional cardiovascular risk factors and metabolic syndrome in predicting carotid intima-media thickness progression in young adults: the cardiovascular risk in young Finns study. Circulation. Jul 21 2009;120(3):229-236.
74. Juonala M, Viikari JS, Kahonen M, et al. Life-time risk factors and progression of carotid atherosclerosis in young adults: the Cardiovascular Risk in Young Finns study. European heart journal. Jul 2010;31(14):1745-1751.
75. Gidding SS, Lichtenstein AH, Faith MS, et al. Implementing American Heart Association pediatric and adult nutrition guidelines: a scientific statement from the American Heart Association Nutrition Committee of the Council on Nutrition, Physical Activity and Metabolism, Council on Cardiovascular Disease in the Young, Council on Arteriosclerosis, Thrombosis and Vascular Biology, Council on Cardiovascular Nursing, Council on Epidemiology and Prevention, and Council for High Blood Pressure Research. Circulation. Mar 3 2009;119(8):1161-1175.
76. McGill HC, Jr., McMahan CA, Zieske AW, Malcom GT, Tracy RE, Strong JP. Effects of nonlipid risk factors on atherosclerosis in youth with a favorable lipoprotein profile. Circulation. Mar 20 2001;103(11):1546-1550.
77. Elgharib N, Chi DS, Younis W, Wehbe S, Krishnaswamy G. C-reactive protein as a novel biomarker. Reactant can flag atherosclerosis and help predict cardiac events. Postgraduate medicine. Dec 2003;114(6):39-44; quiz 16.
78. Labarrere CA, Zaloga GP. C-reactive protein: from innocent bystander to pivotal mediator of atherosclerosis. The American journal of medicine. Oct 1 2004;117(7):499-507.
79. Hashimoto H, Kitagawa K, Hougaku H, et al. C-reactive protein is an independent predictor of the rate of increase in early carotid atherosclerosis. Circulation. Jul 3 2001;104(1):63-67.
80. Hashimoto H, Kitagawa K, Hougaku H, Etani H, Hori M. C-reactive protein predicts carotid atherosclerosis progression in mild to moderate risk and middle-aged patients. Clinical and investigative medicine. Medecine clinique et experimentale. Apr 2006;29(2):77-82.
81. Toprak A, Kandavar R, Toprak D, et al. C-reactive protein is an independent predictor for carotid artery intima-media thickness progression in asymptomatic younger adults (from the Bogalusa Heart Study). BMC cardiovascular disorders. 2011;11:78.
82. Bisoendial RJ, Boekholdt SM, Vergeer M, Stroes ES, Kastelein JJ. C-reactive protein is a mediator of cardiovascular disease. European heart journal. Sep 2010;31(17):2087-2091.
83. Ridker PM, Rifai N, Rose L, Buring JE, Cook NR. Comparison of C-reactive protein and low-density lipoprotein cholesterol levels in the prediction of first cardiovascular events. The New England journal of medicine. Nov 14 2002;347(20):1557-1565.
84. Chiuve SE, McCullough ML, Sacks FM, Rimm EB. Healthy lifestyle factors in the primary prevention of coronary heart disease among men: benefits among users and nonusers of lipid-lowering and antihypertensive medications. Circulation. Jul 11 2006;114(2):160-167.
85. Pruchno RA, Wilson-Genderson M, Cartwright F. A two-factor model of successful aging. The journals of gerontology. Series B, Psychological sciences and social sciences. Nov 2010;65(6):671-679.
86. Hitt R, Young-Xu Y, Silver M, Perls T. Centenarians: the older you get, the healthier you have been. Lancet. Aug 21 1999;354(9179):652.
87.Friedmann PD, Brett AS, Mayo-Smith MF. Differences in generalists? and cardiologists? perceptions of cardiovascular risk and the outcomes of preventive therapy in cardiovascular disease. Annals of internal medicine. Feb 15 1996;124(4):414-421.
88. Grover SA, Lowensteyn I, Esrey KL, Steinert Y, Joseph L, Abrahamowicz M. Do doctors accurately assess coronary risk in their patients? Preliminary results of the coronary health assessment study. BMJ. Apr 15 1995;310(6985):975-978.
89. Vancheri F, Strender LE, Montgomery H, Skaner Y, Backlund LG. Coronary risk estimates and decisions on lipid-lowering treatment in primary prevention: comparison between general practitioners, internists, and cardiologists. European journal of internal medicine. Oct 2009;20(6):601-606.
90. Sposito AC, Ramires JA, Jukema JW, et al. Physicians? attitudes and adherence to use of risk scores for primary prevention of cardiovascular disease: cross-sectional survey in three world regions. Current medical research and opinion. May 2009;25(5):1171-1178.
verlander verlander justin verlander pepper spraying cop pepper spraying cop somaya reece juelz santana
No comments:
Post a Comment
Note: Only a member of this blog may post a comment.